Shop By Category
Browse by Health Conditions


Live Healthy
Powered by

EFFORTLESS ONLINE MEDICINE ORDERS AT APOLLO PHARMACY
Because ordering medicines online need not be complicated but rather a cakewalk. And at Apollo Pharmacy we ensure that. All you need to do is:
- Browse through our wide variety of products
- Add products to your cart and complete the payment. Voila!
- Your order will be on its way to you.
Apollo Pharmacy is your go-to online pharmacy store for all your medicine needs. We also have a range of products in the personal care, baby care, health and nutrition, wellness, and lifestyle categories. Come explore ‘everything under the sun’ related to healthcare at Apollo Pharmacy.
Reasons To Buy Medicine From Apollo Pharmacy
For over 39 years, Apollo Pharmacy has been providing you with genuine medicines round-the-clock, through 24-hour pharmacies. And now through Apollo Pharmacy, we intend to make your lives easier – by getting your medicines delivered to you. Yes, no more stepping out to get your medicines, no more standing in long queues, no more worrying about the genuineness of medicines, no more sweat! Here are more reasons why you should buy your medicines from Apollo Pharmacy:
- Super-fast deliveries. In select cities, deliveries are done in as less as 1 day
- Largest pharmacy chain in India with over 5,600 stores
- Attractive deals on medicines and other FMCG products
- Get Health Credits on purchases (not applicable on discounted products)
- Option to consult with a pharmacologist to check medicine interactions
- Wide range of healthcare products to choose from
- Only genuine and top-quality products delivered.
Apollo Pharmacy - Largest Online Pharmacy In India
With more than 5,600 stores in India, Apollo Pharmacy is not just the largest online pharmacy store in India but in Asia as well. Our pharmacy chain has been operational and been providing genuine quality healthcare products for more than 39 years. Our wide range of products ensures that everything you need related to healthcare, you will find it on our platform.
Most Trusted Online Medical Store Of India
As pioneers in the healthcare segment, we understand the importance of trust. And that is why, over the years, we worked on building that trust. We ensure that every product sold through our offline/online stores are checked for their authenticity, quality, and compliance with the Central Drugs Standard Control Organization, the national regulatory body for Indian pharmaceuticals and medical devices.
100% Genuine Medicine From Apollo Pharmacy
All medicines/healthcare products sold on Apollo Pharmacy are procured from our sister company - Apollo Pharmacy, with a reputation of selling only 100% genuine products. The products sold through Apollo Pharmacy are inspected thoroughly to ensure only genuine products make the cut. We believe that when it comes to medicines, quality and authenticity should never be compromised.
Over 5,600 Pharmacy Stores In India
Our strong network lets us deliver medicines to every nook and corner of the country. We have more than 5,600 pharmacy stores in India catering to all your medicine needs. Our network is so vast that you may find an Apollo Pharmacy store at every 1 km. We are leveraging this vast network to now become an online medical store – by getting these medicines delivered to you.
Fastest Home Delivery Of Your Order
When it comes to medicines, most of us do not want to take a chance. This is why most of us prefer going to a store physically to get medicines. But you know what happens at the stores. First, you need to go there physically which means you have to drive/walk/ride for at least 10-15 minutes. Second, you need to wait for your turn which may come after 10-15 minutes. Third, you can only buy the products you are sure about. What if you want to buy an FMCG product but are not sure which one? You cannot expect the pharmacist to give you too many options.
Apollo Pharmacy is the solution to all these. We deliver the medicines to you without you having to step out or wait in the queue to buy medicines. And we give you the option to browse through a variety of non-pharma products to choose from.
Are we missing something here? Yes, the time we take to deliver your order. We understand that you may sometimes require medicines in urgency and that is why we assure you the fastest home delivery of your medicines. Also, depending on the city you reside in, medicines can be delivered in as less as 1 hour.
Extra Benefits Of Online Medicine Orders
When you order medicines at Apollo Pharmacy, not only do you get your medicines delivered on time and at your doorstep, but you also get additional benefits. You can earn Apollo Health Credits whenever you order medicine online and also when you purchase other non-pharma products (not applicable on discounted products including the ones where coupon codes have been applied). You can use these Health Credits to make more purchases on our platform. And not to forget the discounts and exclusive offers we bring out from time to time.
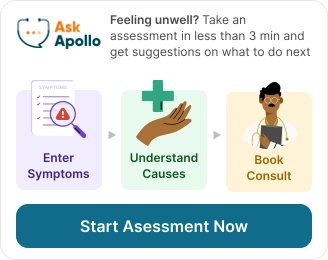
Additional Services I Will Receive
Besides purchasing medicines, the additional services you can avail on our platform are doctor consultations, symptom checker, ordering diagnostic tests, and digitization of your health records. These services let you consult with doctors from over 70 specialties, check and understand your symptoms, book diagnostics tests, and convert your physical health records into digital records. With so many services under our umbrella, you wouldn’t need to go anywhere else.
Frequently asked questions
Ordering medicines from Apollo Pharmacy online medical store is quick and hassle-free. If you wish to purchase over-the-counter medicines or FMCG products, all you need to do is click on the ‘Buy Medicines’ section on the app/website and type the name of the product you wish to buy in the search box. Once you select the product, you can click on the ‘Add to Cart’ button and proceed to make the payment. Once your order has been confirmed, we will start prepping your order for home delivery.
Absolutely! All the medicines/products sold through our platform are inspected thoroughly for their authenticity and quality. Also, while delivering the medicines, our team follows strict safety protocols to ensure only the top-notch products get delivered to you.
If, for any reason, your order is delayed, our team will contact you either through SMS, call or email and inform you of the same. You can also check the status of your order on the app/website by clicking on the ‘Order Status’ button.
Yes, depending on the city you reside in. In select cities, orders are delivered in as less as 1 hour. Please note that the express deliveries may be based on various other factors such as medicine availability, availability of the staff, etc.
Besides walking into an Apollo Pharmacy outlet and buying the medicines in person, you can purchase products from Apollo Pharmacy on the Apollo Pharmacy app or website. To do this, you will need to visit the app/website of Apollo Pharmacy and click on the ‘Buy Medicines’ section.
To track your order, you can click on the ‘My Orders’ section under the ‘My Account’ tab. Then click on the particular order to check the status of your order.
Yes, Apollo Pharmacy provides the fastest home delivery of medicines.
Yes, Apollo Pharmacy provides same day delivery of online medicine order.