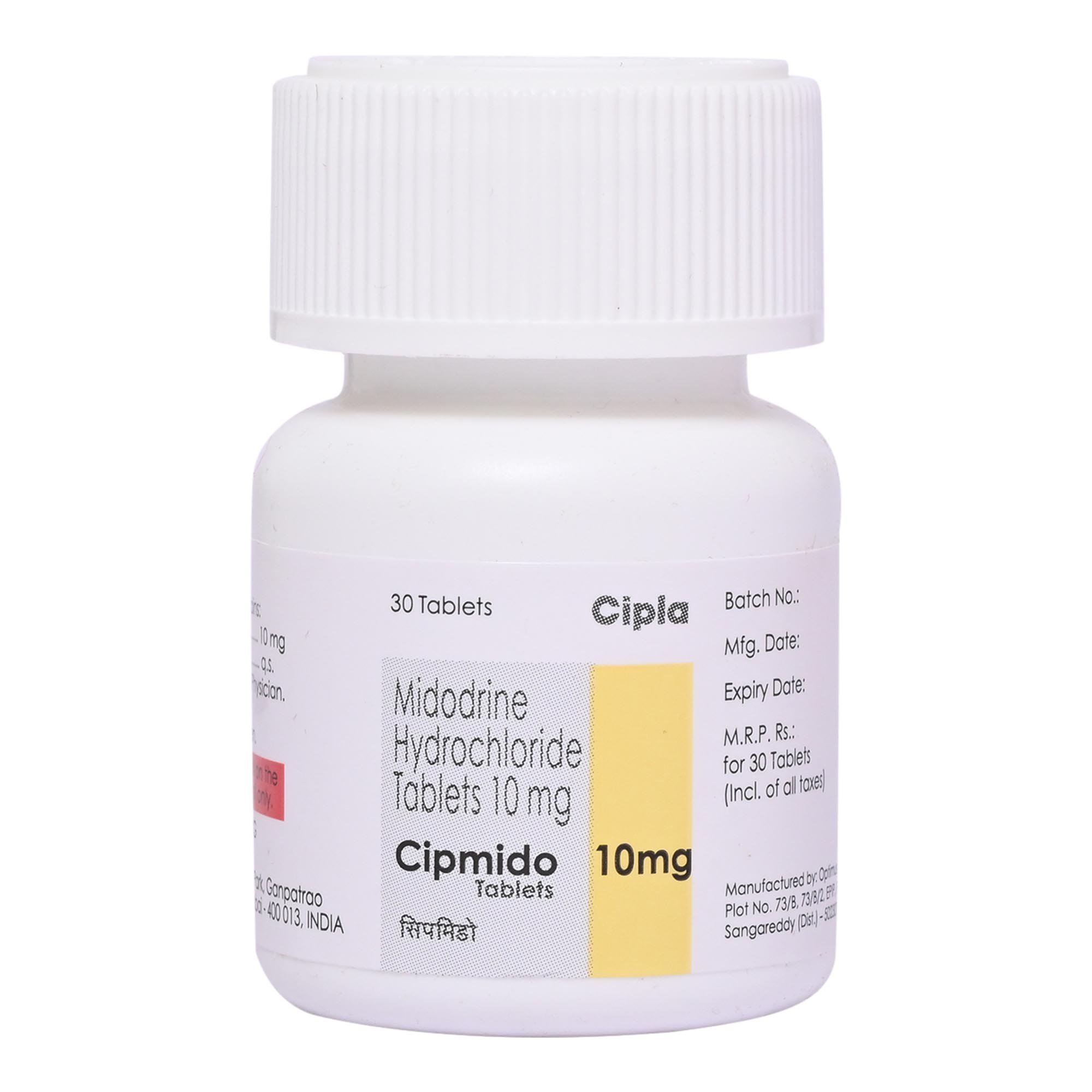
Midodrine
About Midodrine
Midodrine belongs to a group of medicines called antihypotensives, which are used to treat low blood pressure (hypotension). Low blood pressure is when blood flow drops below normal, which can cause dizziness, weakness, fainting, and increase the risk of falls.
Midodrine contains midodrine hydrochloride, which works on blood vessels through the nervous system to improve blood flow. This helps relieve symptoms like dizziness, fainting, blurred vision, and weakness when sitting or standing up.
Some people may experience supine hypertension, reflex bradycardia, arrhythmias, rash, nausea, vomiting, dyspepsia, headache, and urinary retention. Most of these side effects of Midodrine do not require medical attention and gradually resolve over time. However, if the side effects persist or worsen, please consult your doctor.
Midodrine is contraindicated in patients with severe organic heart disease, congestive heart failure, thyrotoxicosis, phaeochromocytoma, acute renal disease, severe renal insufficiency, urinary retention, narrow-angle glaucoma, hyperthyroidism, or known hypersensitivity to any component of the product. Inform your doctor if you are a pregnant woman or nursing mother.
Uses of Midodrine
Medicinal Benefits
- Midodrine contains midodrine hydrochloride, which acts on the blood vessels via the sympathetic nervous system to correct imbalances of blood distribution.
- Midodrine helps to prevent symptoms like weakness, blurred vision, and fatigue caused by sudden drops in blood pressure.
- Supports better daily functioning and safety by reducing the risk of falls related to low blood pressure.
Directions for Use
- Midodrine can be taken with meals.
- It is usually taken 2-3 times daily during the daytime, with each dose taken 3 hours apart, or as prescribed by your doctor.
- Swallow Midodrine as a whole with a glass of water.
- Do not crush, chew, or break it.
Storage
Side Effects of Midodrine
- Supine hypertension
- Chest pain
- Palpitations
- Headache
- Blurred vision
- Reflex bradycardia
- Arrhythmias
- Rash
- Nausea
- Vomiting
- Dyspepsia
- Urinary retention
Drug Warnings
- If you are known to be allergic to Midodrine or any other medicines, please tell your doctor.
- If you are pregnant or breastfeeding, think you may be pregnant, or are planning to have a baby, ask your doctor for advice before taking this medicine.
- Midodrine should not be used by children below 18 years.
- Midodrine is contraindicated in patients with severe organic heart disease, congestive heart failure, thyrotoxicosis, pheochromocytoma, acute renal disease, severe renal insufficiency, urinary retention, narrow-angle glaucoma, and hyperthyroidism.
- Inform your doctor if you have a history of stroke (CVA); close monitoring may be needed.
- Avoid driving or operating heavy machinery if you feel dizzy or lightheaded.
- Do not stop taking Midodrine suddenly without consulting your doctor.
- Midodrine can cause high blood pressure when lying down, so regular blood pressure checks are important.
Drug Interactions
Drug-drug interactions: Midodrine may interact with drugs used to treat depression and anxiety (e.g. duloxetine), medicines used to help control the amount of sodium and fluids in your body (e.g. fludrocortisone), and medications used to treat high blood pressure (e.g. metoprolol).
Drug-food interactions: Consuming alcohol with Midodrine is not advisable as it may cause unpleasant side effects.
Drug-disease interactions: Midodrine should be used with caution in patients with heart disease/ hypertensive effects, kidney or liver dysfunction and diabetes.
Drug-Drug Interactions Checker List:
Safety Advice
Alcohol
unsafeConsuming alcohol along with Midodrine is not advisable as it may cause unpleasant side effects.
Pregnancy
consult your doctorPlease consult the doctor. There are no adequate and well-controlled studies on pregnant women.
Breast Feeding
consult your doctorConsult your doctor, and there is no substantial research yet on the use of Midodrine in breastfeeding/nursing mothers.
Driving
unsafeIf you feel dizzy or lightheaded while taking Midodrine, avoid driving or using machines.
Liver
consult your doctorLimited information is available on the use of Midodrine in patients with liver disease. Please consult your doctor.
Kidney
consult your doctorLimited information is available on the use of Midodrine in patients with Kidney disease. Please consult your doctor.
Children
unsafeMidodrine is not recommended for children below 18 years of age.
Habit Forming
Diet & Lifestyle Advise
- Add foods with high vitamin B12, including eggs, fortified cereals, and nutritional yeast, to your daily diet.
- Salty foods can increase blood pressure. Try eating canned soup, cottage cheese, olives, and pickled items.
- Drink coffee and caffeinated tea, which may increase blood pressure by stimulating the cardiovascular system.
- Eat small meals more frequently; large meals may drop in blood pressure as your body works harder to digest larger meals.
- Drink more water and limit alcohol; dehydration lowers blood pressure.
- Change body position by standing up slowly.
- Avoid prolonged bed rest.
- If you exercise outdoors in extreme heat, take frequent breaks.
- Avoid spending a long time in saunas, hot tubs, and steam rooms, which cause dehydration.
Patients Concern
Disease/Condition Glossary
Hypotension: Low blood pressure occurs when blood pressure drops below the normal range. It can cause dizziness, weakness, fainting, and the risk of injury from falls. Also, severely low blood pressure can deprive your body of enough oxygen to carry out its functions, damaging your heart and brain. Systolic pressure is the pressure when the heart pumps blood out. On the other hand, diastolic pressure is the pressure in the arteries when the heart rests between heartbeats. Ideal blood pressure should be 120/80 mmHg. Hypotension exists when the systolic pressure is less than 90 mmHg and the diastolic pressure is less than 60 mmHg.
FAQs
Midodrine is used to treat idiopathic postural hypotension or hypotension (low blood pressure)
Midodrine contains the active ingredient midodrine hydrochloride, which acts on the blood vessels via the sympathetic nervous system to correct imbalances of blood distribution. This should help relieve the symptoms you might suffer, such as dizziness, fainting, blurred vision, and weakness when sitting or standing up.
Do not stop taking Midodrine on your own. Depending on your medical condition, you are advised to take Midodrine for as long as your doctor has prescribed it for you. Do not hesitate to speak with your doctor if you experience difficulty while taking Midodrine.
Midodrine is contraindicated in patients with severe organic heart disease, congestive heart failure, thyrotoxicosis, phaeochromocytoma, acute renal disease, severe renal insufficiency, urinary retention, narrow-angle glaucoma, hyperthyroidism, known hypersensitivity to any component of the product. And also, Patients with a history of CVA should be monitored closely.
Midodrine is metabolised to desglymidodrine, an active metabolite that activates alpha-1-adrenergic receptors on arterioles and venules, causing smooth muscle contraction and blood pressure increase. Midodrine may cause a drop in heart rate due to the vagal reflex.
The side effects of Midodrine include nausea, vomiting, indigestion, supine hypertension (high blood pressure while lying down), and dysuria (painful or uncomfortable urination). If these side effects persist or worsen, please consult your doctor.
Yes, Midodrine may cause high blood pressure when you are lying flat on your back (supine hypertension). Midodrine should only be used by people whose low blood pressure affects their daily activities and in people who could not be treated successfully with other therapies.
You are advised not to lie down immediately after taking Midodrine due to the risk of supine hypertension (high blood pressure when you are lying flat on your back). Therefore, it is recommended to take the final dose of the day at least 4 hours before bedtime. By elevating the head, you can reduce the risk of supine hypertension during the night.
Midodrine may take about 1 hour to show its effects. Though the effect lasts for about 2-3 hours, the action lasts for a short time only.
Take Midodrine exactly as advised by your doctor. It is taken orally with or without food. Swallow it as a whole with a glass of water. Do not break, crush or chew it.
Midodrine is not recommended for patients who are allergic to any of its components, who have unusually slow heart rate, severe heart disease, high blood pressure, conditions causing tightening of the arteries, urinary retention (when the bladder cannot empty properly), overactive thyroid, enlarged prostate gland, pheochromocytoma (tumour of the adrenal medulla), acute or severe kidney disease, poor vision as a result of diabetes and narrow-angle glaucoma (elevated pressure in the eye).
Before starting Midodrine, you may need to get your liver and kidney function tests done and check your blood pressure. After starting the treatment, keep a constant track of your heart rate and blood pressure, especially after lying down.
Symptoms of supine hypertension include shortness of breath, chest pain, palpitations (abnormalities of heartbeat), blurred vision, and headache. If you develop these symptoms, consult your doctor immediately. The doctor may lower the dose of Midodrine or discontinue treatment if the symptoms persists.
You should be cautious while using Midodrine and metoprolol together as it can decrease your heart rate significantly. If you experience dizziness, fainting and slow pulse, inform your doctor as the dose of these medicines may need to be adjusted. However, please consult your doctor before using other medicines with Midodrine.