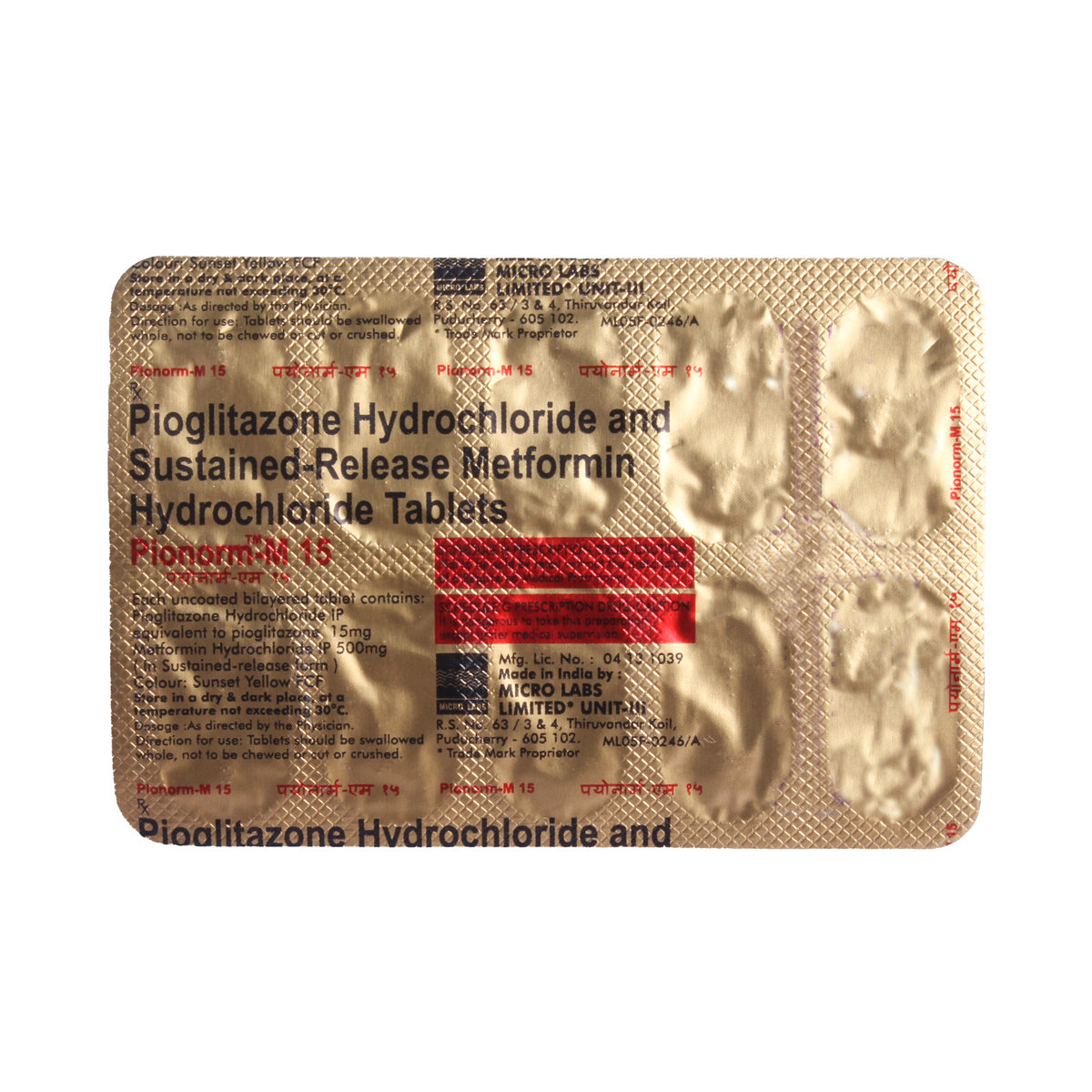
Pioglitazone+metformin
About Pioglitazone+metformin
Pioglitazone+metformin is used to treat type 2 diabetes. Type 2 diabetes develops when the body either does not produce enough insulin or when the insulin produced does not work properly.
Pioglitazone+metformin contains Pioglitazone and Metformin. Pioglitazone lowers blood sugar by helping body cells to take up free glucose from the blood. Metformin decreases blood sugar levels by reducing its formation and increasing its utilisation by cells.
Some people may experience stomachaches, nausea, vomiting, diarrhoea, loss of appetite, localised swelling (oedema), weight gain, headaches, respiratory infections, numbness, and taste disturbances. Most of these side effects do not require medical attention. However, talk to your doctor if you experience these side effects persistently.
Pioglitazone+metformin should not be stopped without your doctor’s advice, as suddenly stopping it can raise sugar levels and increase the risk of eye, kidney, and nerve damage. Please inform your doctor if you have any heart disease, are planning to get pregnant, or are breastfeeding.
Uses of Pioglitazone+metformin
Medicinal Benefits
- Pioglitazone+metformin is used in adults to treat type 2 (non-insulin-dependent) diabetes mellitus when treatment with metformin alone is not sufficient.
- Pioglitazone+metformin plays a vital role in controlling blood sugar levels and prevents serious complications of diabetes like eyesight loss (retinopathy), kidney (nephropathy), nerve damage (neuropathy), diabetic foot ulcer and delayed wound healing.
- Pioglitazone+metformin lowers blood sugar by activating cell switches (PPAR) to take up free glucose from the blood and use it for energy production, and decreases the production of glucose inside the liver.
Directions for Use
- Pioglitazone+metformin should be taken with food to avoid an upset stomach.
- It should be taken at the same time of the day each time for the best results.
- Swallow it as a whole with a glass of water.
- Do not crush, chew, or break it.
Storage
Side Effects of Pioglitazone+metformin
- Diarrhoea
- Loss of appetite
- Headache
- Nausea
- Vomiting
Drug Warnings
- Pioglitazone+metformin should not be used in patients with type 1 diabetes or with diabetic ketoacidosis.
- A few diabetic patients, while taking Pioglitazone+metformin, might develop a rare but serious condition called lactic acidosis. In this condition, too much lactic acid accumulates in the blood, which can damage the liver and kidneys, the organs responsible for eliminating excess lactic acid from the blood.
- Before you start taking Pioglitazone+metformin, tell your doctor if you’ve ever had pancreatitis (inflammation of the pancreas), kidney disease, or low vitamin B12 levels. Pioglitazone+metformin, when used with insulin, may extremely lower the blood sugar level, leading to a hypoglycemia condition, which can be fatal.
- Prolonged intake of Pioglitazone+metformin may lower your thyroid-stimulating hormone (TSH); therefore, an annual TSH check-up is recommended.
- In rare cases, you may also develop a serious skin reaction known as bullous pemphigoid that requires immediate medical attention.
- Inform your doctor if you are scheduled to undergo a diagnostic test that involves an injection of dye or an X-ray contrast agent. The use of Pioglitazone+metformin should be stopped for a short time before having an X-ray procedure.
Drug Interactions
Drug-Drug Interaction: Pioglitazone+metformin interacts with heart medications like (propranolol), pain killers (aspirin, ibuprofen, and celecoxib), high blood pressure-lowering pills (nifedipine, captopril, enalapril, lisinopril), thyroid hormones (thyroxine), antacids (cimetidine), or certain medicines affecting the nervous system.
Drug-Food Interaction: Intake of excessive alcoholic beverages may increase the chance of a life-threatening condition known as Lactic Acidosis. So, avoid intake of alcoholic beverages with Pioglitazone+metformin.
Drug-Disease Interaction: People affected with heart, liver, and kidney diseases (like congestive heart failure and myocardial infarction), vitamin B12 deficiency, and alcoholism should avoid intake of Pioglitazone+metformin.
Drug-Drug Interactions Checker List:
Safety Advice
Alcohol
unsafeNot recommended with alcohol as it may result in a harmful decrease or increase in levels of blood sugar depending on how much alcohol a patient has consumed.
Pregnancy
cautionNot recommended in pregnancy. Pioglitazone+metformin treatment should be stopped and replaced with any other alternative drug from other blood sugar-lowering agents on the recommendation of a doctor. You must tell your doctor if you are pregnant, think you may be pregnant or are planning to have a baby.
Breast Feeding
cautionNot recommended for breastfeeding mothers. Do not use Pioglitazone+metformin if you are breastfeeding or are planning to breastfeed, as a doctor's consultation is required.
Driving
safe if prescribedIt is safe to use while driving or operating heavy machinery. This medicine will not affect your ability to drive or use machines, but care should be taken if you experience abnormal vision or anything that affects your ability to drive.
Liver
cautionPioglitazone+metformin should be used with caution in patients with liver disease, as Pioglitazone+metformin has been found to cause harmful interactions in them. A doctor's recommendation is required before taking this drug.
Kidney
cautionPioglitazone+metformin should be taken with caution in patients with kidney disease. In rare cases, serious interactions have been found in kidney patients, called lactic acidosis; thus, a doctor's consultation is required before taking this drug.
Children
unsafePioglitazone+metformin is not recommended for use in children and adolescents under 18 years. Talk to your doctor for better alternative blood sugar-lowering agents in diabetic children.
Habit Forming
Diet & Lifestyle Advise
- Fill your half plate with starchy veggies, a quarter with proteins, and a quarter with whole grains.
- Eat at regular intervals. Do not leave a long gap between meals or snacks.
- Monitor your blood sugar level regularly, especially when there are lots of fluctuations.
- Invest in at least 150 minutes of moderate-intensity physical activity or one hour and 15 minutes of high-intensity exercise every week.
- Lose weight gradually to achieve a healthy body mass index (18.5 to 24.9).
- Replace refined carbohydrate-containing foods with whole-grain foods and increase your intake of fruits, vegetables, and other fibre-enriched foods.
- Reduce your intake of saturated fat (or hidden fats) in foods like chips, crisps, pastries, biscuits, and samosas. Choose omega-3 fatty acid-containing oils for daily cooking. For frying, you can use palm oil, mustard oil, groundnut oil, rice bran oil, and safflower oil.
- Do not take stress as it may elevate your blood sugar level. You can adopt stress management techniques, such as mindfulness, to help control stress-related blood sugar changes.
- Opt for low-fat dairy products (low-fat yoghurt, fat-free milk, and cheese, etc.).
- Keep your blood pressure as normal (140/90) as possible. As it reduces the risk of cardiovascular diseases in diabetes patients.
Special Advise
- Contact your doctor immediately if you have nausea, vomiting, Kussmaul breathing (laboured and deep), and generalised weakness, which are symptoms of Lactic acidosis, a very rare but serious metabolic complication.
Patients Concern
Disease/Condition Glossary
Type 2 diabetes is a condition where the body is unable to make sufficient insulin, or the insulin that it makes doesn't work properly or is utilised by the body. This can cause high blood sugar levels (hyperglycaemia). Symptoms of type 2 diabetes include increased thirst, frequent urination, slow, increased hunger, fatigue, and blurred vision. In some cases, weight gain may occur, while in rare instances, weight loss may be observed. The complication of type 2 diabetes also includes neuropathy (nerve problems), nephropathy (kidney problems), retinopathy (damaged retina of the eyes or blindness), loss of limbs, sexual dysfunction, and an increased chance of heart attack or stroke.
FAQs
Pioglitazone+metformin is used to treat Type II diabetes (non-insulin-dependent diabetes). It lowers blood sugar by activating cell switches (PPAR) to take up free glucose from the blood and use it for energy production. It also decreases the production of glucose in the liver.
Pioglitazone+metformin can cause fluid retention, which can cause heart failure. The doctor usually recommends starting from a lower dose and increasing the dose slowly while treating patients who are at risk of heart failure. Heart failure is reported mainly in patients taking insulin Pioglitazone+metformin simultaneously.
There have been rare cases of liver damage in patients taking Pioglitazone+metformin. The doctor usually screens the patient continuously during the course of treatment with Pioglitazone+metformin. A patient is advised to visit a doctor strictly as per the doctor's advice.
Pioglitazone+metformin is contradictory when used in patients with high blood pressure. A doctor's consultation is required before taking this drug in a patient with high blood pressure.
Pioglitazone+metformin is safe to take before driving a vehicle or operating machinery, provided blood sugar levels are stable. However, a patient is advised to take proper precautions and make sure that Pioglitazone+metformin is not taken with another blood sugar-lowering agent.
Not recommended to be taken with contraceptives. Pioglitazone+metformin decreases the activity of oral contraceptives like Ethinyl estradiol by almost 30% and leads to failure of contraception.
Type 2 diabetes is a condition where the body is unable to produce sufficient insulin, or the insulin it produces doesn't work correctly or is not utilised by the body. This can cause high blood sugar levels (hyperglycemia). Symptoms of type 2 diabetes include increased thirst, frequent urination, slow, increased hunger, fatigue, and blurred vision.
Pioglitazone+metformin should be swallowed as a whole with a glass of water. Avoid crushing, chewing, or breaking it.
Don't stop taking Pioglitazone+metformin without consulting your doctor, even if your blood sugar levels return to normal. Stopping the medication suddenly can cause your blood sugar levels to fluctuate, leading to potential complications. Your doctor prescribed Pioglitazone+metformin to help manage your type 2 diabetes, and they need to assess your condition before making any changes to your treatment plan. Consult your doctor before stopping or adjusting your medication, as they will provide personalised guidance to ensure your blood sugar levels remain stable and under control.
Avoid or limit alcohol consumption while taking Pioglitazone+metformin, as it can interact with the medication and increase the risk of low or high blood sugar levels, as well as a rare but serious condition called lactic acidosis. Additionally, alcohol can worsen certain health conditions, such as nerve damage or liver disease. If you do choose to drink alcohol, do so in moderation and closely monitor your blood sugar levels.
Common side effects of Pioglitazone+metformin may include stomach aches, feeling sick (nausea), vomiting, diarrhoea, loss of appetite, localised swelling (oedema), weight gain, headache, respiratory infection, numbness, taste disturbance, etc. Most of these side effects of Pioglitazone+metformin do not require medical attention and typically resolve on their own over time. However, if the side effects persist or worsen, please consult your doctor.
To make an informed decision, consult your healthcare professional, who can assess your individual situation and provide personalised guidance on using Pioglitazone+metformin while breastfeeding.
Pioglitazone+metformin should be taken with caution in patients with kidney disease. In rare cases, serious interactions have been found in kidney patients, called lactic acidosis; thus, a doctor's consultation is required before taking Pioglitazone+metformin.
Pioglitazone+metformin is recommended not to be used in children. Pioglitazone+metformin is a medication typically prescribed for adults over 18 years with type 2 diabetes.
Pioglitazone+metformin is not recommended during pregnancy as there is not much information about its safety during pregnancy. If you are pregnant or thinking of getting pregnant, talk to your doctor, as they will need to review your treatment. They can suggest a different medicine that is safer for you to take during pregnancy.
Store in a cool and dry place away from sunlight. Keep Pioglitazone+metformin out of reach and out of sight to children.
No, Pioglitazone+metformin is not indicated for treating type 1 diabetes. Pioglitazone+metformin is a medication specifically designed to treat type 2 diabetes, and it's not suitable for managing type 1 diabetes.
Pioglitazone+metformin can interact with various other drugs, including those used to manage diabetes, blood pressure, heart conditions, and thyroid disorders, as well as steroids and blood thinners. Always let your healthcare professional know about all the medications you are currently taking to reduce risks. They will help you navigate potential interactions and ensure safe treatment. Consulting your healthcare professional before combining Pioglitazone+metformin with any other medications is key.
Pioglitazone+metformin contains Pioglitazone (thiazolidinedione) & Metformin (biguanide).